Non Vacuum Tubes in Modern Healthcare: A Safer, Smarter Approach to Blood Collection
Accurate and efficient blood collection is the bedrock of diagnostic medicine. While vacuum tubes dominate routine phlebotomy, there are numerous situations where a more controlled and manual method is required. Enter the non vacuum tube, a simple yet powerful tool that enables clinicians to collect blood specimens safely, precisely, and effectively. Especially valuable in pediatrics, geriatrics, emergency scenarios, and specialized testing, non vacuum tubes provide flexibility and control that vacuum systems cannot match. As healthcare systems emphasize patient safety and specimen integrity, the non vacuum tube continues to prove its worth. In this article, Kangjian explores the benefits of non vacuum tubes in medical environments, providing detailed insights for clinical decision-makers, procurement managers, and laboratory professionals.
What Is a Non Vacuum Tube?

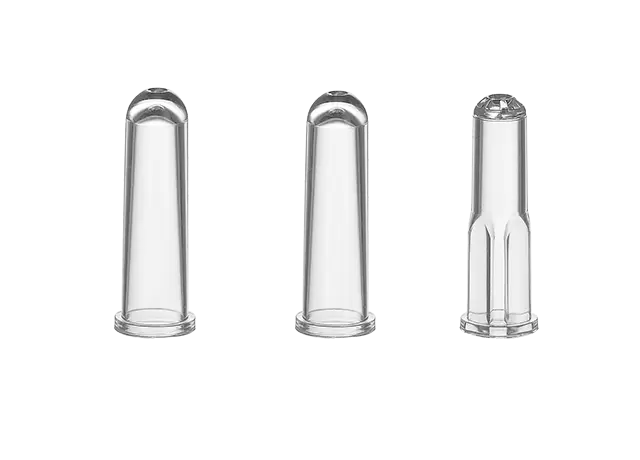
A non vacuum tube is a sterile blood collection container without internal negative pressure. It relies on manual blood transfer via syringe, as opposed to automatic suction-based draw. The design consists of a chemically treated or untreated tube with a secure, color-coded cap and pre-measured additives such as EDTA, sodium citrate, or clot activators.
Blood is first drawn into a syringe from the patient and then carefully dispensed into the tube, maintaining control over flow rate and pressure. This minimizes the risk of vein collapse, hemolysis, and specimen damage. Non vacuum tubes can be made from medical-grade PET or borosilicate glass, both capable of withstanding centrifugation and temperature variation. These tubes are commonly used in conjunction with special transfer devices or closed systems to preserve sterility and prevent cross-contamination.
Their compatibility with laboratory instruments and analyzers makes them fully functional in modern hospital labs, even without automation. With clearly printed labels, writable areas, and traceable barcodes, non vacuum tubes integrate well into digital medical record systems and laboratory workflows.
Key Benefits of Non Vacuum Tubes in Clinical Practice
The value of non vacuum tubes lies not only in their basic ability to collect blood but also in the multifaceted clinical advantages they bring compared to conventional vacuum-based systems. These advantages are particularly evident in patient-centered care, sample quality assurance, cost-effective clinical operations, and adaptability across diverse healthcare scenarios. In both high-tech urban hospitals and low-resource field clinics, non vacuum tubes demonstrate significant value in supporting accurate diagnostics and improving the patient experience. Below, we explore these benefits in detail.
Patient Comfort and Safety
One of the foremost benefits of using non vacuum tubes is the improved comfort and safety they offer during venipuncture procedures. Because blood is drawn manually—typically with a syringe and then transferred into the tube—the healthcare provider can regulate the flow rate and amount of suction applied. This is especially beneficial for patients with fragile, rolling, or shallow veins, such as infants, the elderly, or patients undergoing long-term treatments that involve frequent blood draws.
The gentle collection method reduces the likelihood of vein collapse, hematoma formation, and post-procedure bruising. In contrast, vacuum tubes exert immediate negative pressure that can sometimes cause veins to rupture or collapse, especially in dehydrated or hypotensive patients. The non vacuum tube provides a more patient-sensitive approach, allowing clinicians to adapt the technique to the patient's condition in real time. This leads to higher patient satisfaction, fewer repeat punctures, and overall safer blood collection procedures.
In home care and mobile phlebotomy, where patients may already be anxious or physically vulnerable, the non vacuum tube becomes an essential tool for ensuring a low-stress, minimally invasive experience.
Improved Sample Quality
The integrity of the blood sample is critical for accurate laboratory testing. Hemolysis (the rupture of red blood cells), platelet activation, and clotting can significantly distort lab results, leading to misdiagnosis, test repetition, or delayed treatment. Non vacuum tubes greatly reduce these risks by allowing manual transfer of blood into the tube, thereby minimizing the mechanical stress and turbulence that can damage cells.
The slower, more controlled entry of blood into the non vacuum tube limits bubble formation, reduces shear forces, and preserves the natural state of blood components. This is particularly important for tests measuring potassium, liver enzymes, cardiac markers, or coagulation parameters, where even slight hemolysis can skew results.
Furthermore, with proper mixing of additives through gentle inversion, the non vacuum tube ensures uniform anticoagulation or clot activation, avoiding microclots or fibrin strands that can interfere with automated analyzers. In sensitive assays such as hormone quantification or drug monitoring, the cleaner, more stable sample environment provided by non vacuum tubes contributes directly to diagnostic accuracy and clinical reliability.
Versatile Volume Management
Unlike vacuum tubes, which are pre-evacuated to draw a fixed amount of blood based on internal pressure, non vacuum tubes allow complete freedom in determining the sample volume. This is a critical advantage in personalized and precision-based medicine, where the exact quantity of blood needed may vary from test to test or patient to patient.
In neonatal intensive care units (NICUs), for instance, even small amounts of blood loss can be physiologically significant. Non vacuum tubes empower clinicians to collect only the minimum volume necessary for essential tests, minimizing iatrogenic anemia. Similarly, in geriatric and oncology care, where patients are often fragile and blood draws are frequent, reducing cumulative blood loss is vital for maintaining health and stability.
This flexible volume capability is also helpful in multi-test scenarios, where different assays may require distinct amounts of blood or specific blood-to-additive ratios. A single draw using a non vacuum tube can be carefully divided to meet each test’s needs, improving efficiency while preserving sample quality.
Greater Adaptability for Specialized Testing
Certain laboratory analyses demand precise handling that vacuum systems may not accommodate. For example, coagulation tests require strict control of blood-to-citrate ratios, while hormone and trace metal assays may be sensitive to contaminants or turbulent mixing. The non vacuum tube provides the level of manual control needed to meet these stringent requirements.
In molecular diagnostics and research settings, custom collection protocols are often the norm. A non vacuum tube allows technicians to handle each sample in accordance with the specific protocol—whether that involves layering blood onto separation media, avoiding contact with plasticizers, or introducing anticoagulants at exact time points.
Additionally, non vacuum tubes are frequently used in ESR (erythrocyte sedimentation rate) testing, where a long, narrow tube shape and gentle handling are essential for reproducible results. Because the operator controls every aspect of the collection and mixing process, non vacuum tubes ensure that even the most sensitive diagnostic assays can be executed with high precision.
Reduced Operational Costs
From a procurement and operational standpoint, the non vacuum tube presents a more cost-effective solution for many healthcare systems. Since these tubes do not require internal vacuum generation, their manufacturing process is simpler and less expensive. This cost advantage becomes particularly significant when scaling up for use in national health programs, humanitarian missions, or high-volume clinics.
In addition to lower unit costs, non vacuum tubes require minimal ancillary equipment. There's no need for specialized tube holders, double-ended needles, or vacuum-compatible accessories. A simple syringe and sterile transfer protocol are sufficient, which simplifies logistics and reduces training burdens for staff.
The long shelf life of non vacuum tubes, combined with their chemical and physical durability, also helps reduce waste from expired or damaged stock. In remote or low-resource areas where restocking is difficult, this reliability ensures that essential diagnostic capabilities remain functional over extended periods.
Lastly, by reducing the number of rejected samples due to hemolysis, clotting, or incorrect volumes, non vacuum tubes help avoid the hidden costs associated with re-collection, re-testing, and delayed diagnosis—ultimately improving the cost-efficiency of clinical operations.
While often overshadowed by high-tech laboratory equipment, the non vacuum tube remains a critical component in delivering accurate, safe, and patient-friendly blood collection. It supports clinical outcomes by enabling gentle handling, reducing sample degradation, and ensuring accurate test results across a wide range of medical applications. From hospital labs to field clinics, the role of the non vacuum tube continues to expand. For healthcare providers focused on quality diagnostics, patient safety, and cost efficiency, investing in reliable non vacuum tube systems is not just a procurement decision—it's a strategic move toward better care and precision medicine.